Watch the full interview below or listen to the full episode on your iPhone HERE.
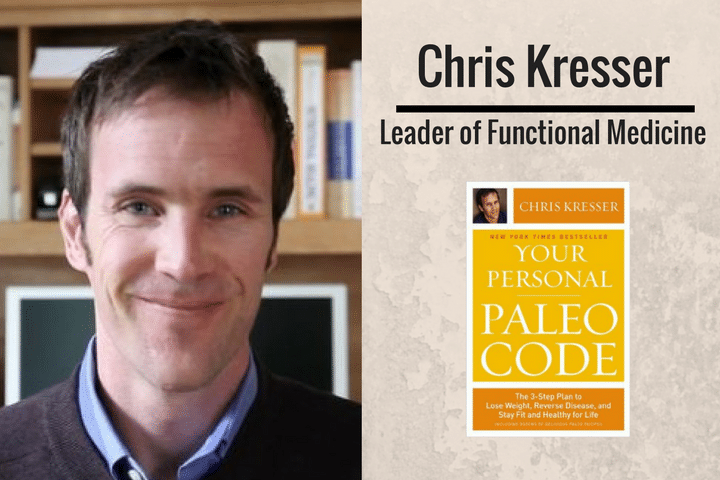
Guy: This week we welcome Chris Kresser to the podcast, he’s a globally recognised leader in the fields of ancestral health, paleo nutrition, and functional / integrative medicine. He is the creator of ChrisKresser.com, one of the top 25 natural health sites in the world, and the author of the New York Times best seller, Your Personal Paleo Code (published in paperback in December 2014 as The Paleo Cure). Chris has been studying, practicing, and teaching alternative medicine for more than fifteen years.
Chris’s work is informed by his own experience recovering from a chronic, complex illness which began while he was traveling in Southeast Asia in his early 20’s. After seeing more than twenty doctors around the world and spending thousands of dollars in an effort to diagnose and treat his condition, Chris decided to take his health into his own hands.
Through extensive study and research, continual self-experimentation, and formal training in integrative medicine, he recovered from this debilitating illness and went on to share what he learned with others through his popular blog, podcast, and private practice.
Use Snapchat? Follow me at: GuyL180 or Click Here.

Audio Version

- What is functional medicine and how does it address those problems?
- How do genes and environmental factors play a part in our longterm health.
- Gut health… is this a buzz word or do we need to carefully consider it.
- What are the fundamental problems with conventional medicine?
- What are your non-negotiables, to be the best version of yourself?
Get More Of Chris Kresser
- https://chriskresser.com/
If you enjoyed this, then you’ll enjoy these interviews with:
- Dr John Hart: Optimizing Brain Function
- Damian Kristof: Blue Zones, Stress Reduction Strategies & Avoiding Nutritional ‘Scare’
180 – Fuelled By Nature
Full range of products HERE.
Leave a Comment
Full Transcript
Guy
Hey, this is Guy Lawrence from 180 Nutrition, and welcome to another awesome episode of The Health Sessions, where of course we’re connecting with as many leading global health and wellness experts around the world to share the best and latest science and thinking, to empower all of us to turn our health and lives around. This week we are doing it with the awesome Chris Kresser.
[00:01:00] I was very excited to get Chris on the show. I’ve been listening to his podcast for quite some time, and he was just the perfect gentleman, a great guy, and insane amount of wealth and knowledge. Myself and Stu picked his brains for an hour and got stuck into all sorts of topics. If you’re not familiar with Chris, he is a globally recognized leader in the fields of functional and integrative medicine. He’s also the creator of Chris Kresser dot com, which is one of the top 25 natural health sites in the world. He is also the author of the New York Times bestselling book, “Your Personal Paleo Code”.
We got into Chris’s own journey, how he got into the functional medicine in the first place, which was driven by his own issues and pain. Then from there, what he’s learned along the way, and from diagnosis, and what exactly is functional medicine, and how we can apply it and how it can help us to live healthier and happier lives as well. I have no doubt you’re going to enjoy the show guys.
[00:02:00] I just wanted to mention as well, if you haven’t been back to our website, 180nutrition.com.au, we’re always updating it, and we’ve updated the actual website only a couple of weeks ago to make it much more user-friendly to find the content that’s in there. We’re constantly adding new products as well, ones that we believe and stand by. Not sure if you knew, but we’ve brought in a [180 Greens Plus 00:01:47] product. That’s been doing fantastically well since we released that. We’ve also brought in L-Glutamine as well, which is designed to help the small intestine, and also help recovery as well and muscle aches. It’s worth getting over there, check out what we got guys, because they’re all there, the tools that we use, and they’re there to design to help you and serve your purpose so we can all improve our nutritional health, and ultimately live a happier life as well. Go back there to 180nutrition.com.au. Anyway, let’s go over to Chris Kresser. Enjoy.
[00:02:30] Hey, this is Guy Lawrence. I’m joined with Stewart Cook as always. Hi Stu. Good to see you there.
Stu
Hello Guy.
Guy
Our awesome guest today is Mr. Chris Kresser. Welcome to the show buddy.
Chris
Hey Guy, Stu. Happy to be here, thanks for inviting me.
Guy
Oh it’s an honor, man.
Stu
Thanks for coming on.
Guy
Yeah, yeah, yeah. We’re big fans of your work, and it’s going to be great to dig in for the next hour, I tell you. What I’ve generally been doing lately, Chris, is asking two questions to kick off the show. The first one’s a short one basically: If a stranger stopped you on the street and asked you what you did for a living, what would you say?
Chris
That really depends on who asks. It’s a tricky question. I’ll typically say that I train clinicians in functional medicine. Then they’ll say, “What the heck is functional medicine,” and we have a conversation about it. That really is how … There are a lot of things that I do, but that’s the thing that I’m most passionate about right now. That would probably be how I’d answer the question today, but six months ago I might have answered it a different way, and maybe in two years I’ll answer it still a different way, we’ll see.
Guy
Perfect mate, perfect. Another, no doubt we’re going to get into the topic of functional medicine at some stage very shortly.
Stu
I hope so.
Guy
Yeah. On top of that mate, can you just take us back what got you into this whole thing in the first place? I know you’ve been on quite a bit of a journey yourself over the years.
Chris
Yeah.
Guy
Yeah, I’d love to get the inside scoop on everything.
Chris
Yeah. We were talking before the show, before we started recording, about surfing. In my early ’20s I took off on a round the world surf trip, and one of the first stops was Indonesia, which I’m sure a lot of your listeners and viewers are familiar with. I get the sense that Indo is kind of like Mexico for us. In California everyone goes to Mexico on surf trips, and in Australia everyone goes to Indo.
Stu
Definitely.
Chris
[00:05:00] I was on an island called Sumbawa at a place called Lakey Peak, which some surfers in your audience will be familiar with. Some locals there dug a trench between this pool of stagnant water that cows were defecating in and milling around in, and the river. Lakey Peak is a river mouth, so all of that sewage went into the surf break. Myself and a few other guys who were there, including some Aussies, got really sick.
It was a classic tropical illness symptoms; vomiting, diarrhea, delirium. I really don’t remember much of what happened for three days, but actually an Australian friend of mine who was there in the village with me had some antibiotics in his medical kit, and they brought me back from the brink.
[00:06:00] I continued to travel. I went to the Maldives after that, and then to South Africa and Madagascar, and Mauritius. Somewhere around Mauritius about six months later, I was just getting sicker and sicker. I had recovered from that acute episode, but it became clear that I was not well. I had planned to be gone for a year and keep going to South America and work my way back up through Central America home, but I had to cut that short and come back early because of this illness.
[00:06:30] Then over the next ten years actually is what it took me to figure out what was going on, and then gradually make my way back to health. I really got taken to the curb, and had to leave no stone unturned in the process of finding my way back. Despite seeing probably 25 different doctors in three countries, and trying every medication and supplement and special diet that you can imagine, none of it really worked. I had to roll up my sleeves and figure it out myself because I realized that no one was coming to save me, and that I had to take responsibility for it. Nobody cared more about me getting better than me, that was just my personality.
[00:07:30] In the process of doing that, I of course learned a lot, and then people around me started asking me questions because they saw I was improving. I decided to formalize that education, go back to school and study integrative and functional medicine, and turn it into a career because I knew so many other people in my life that, yeah, they weren’t suffering to the extreme that I was, but many other people were just not well. They were not well in a way that conventional medicine could really do anything about. I realized that I wanted to help people who were also suffering from chronic illness recover their health. That’s another way I answer that question you asked me in the beginning.
Stu
[00:08:00] Fantastic. I wanted to ask, Chris, before we get into explaining functional medicine, what do you feel the fundamental problems are right now with conventional medicine? I can see that it’s getting a bit of a rap right now in the media in terms of, there’s not a lot of time. It almost seems to be a one size fits all approach. Blankets of antibiotics being prescribed, and that seems to be causing troubles in itself. What do you think the issues are?
Chris
[00:08:30] Yeah. Let’s start with what’s right and good about conventional medicine. If I get hit by a bus, I wanted to be taken to the hospital. We have some pretty amazing emergency and trauma care, acute level care where we’re starting to be able to reattach limbs, and restore sight to the blind. I was just reading about these microchips that are going to be installed in the eyeball that can actually process visual input. People who are blind and never been able to see could actually be able to at least see in some form.
[00:09:00] There’s incredible stuff happening on that end of the spectrum, but the problem is, we don’t really have healthcare. Whether we’re talking about the US or Australia, what we have is really better called disease management. We essentially wait until people get sick and develop a disease, and then we prescribe drugs that suppress the symptoms of that disease instead of addressing the root cause.
[00:10:00] If we use an analogy, and you have a rock in your shoe, you could take ibuprofen, right, and that would help relieve the pain. You could also just take your shoe off and dump out the rock. Conventional medicine is really prescribing ibuprofen for that proverbial rock in the shoe. If you go to the doctor and you have high blood pressure, what’s going to happen? They’re going to give you a medication to lower your blood pressure. If you have high cholesterol, what’s going to happen? They’re going to give you a medication to lower the cholesterol. They’re not typically going to say, “Why is the blood pressure high in the first place? Why is the cholesterol high, and what can we do about that so that we can address this problem without unnecessary drugs? I would say that is the biggest failure of conventional medicine, is not addressing the root cause of problems, and not even having a framework or understanding of health, and promoting health, rather than just managing disease.
Guy
Yeah, perfect. Flipping it over to functional medicine, how would you describe that basically, and then how does that address the problems that the medical systems aren’t addressing?
Chris
[00:11:00] Right. There are a lot of things we could say about functional medicine and how it’s different than conventional medicine, but I’ll just focus on three of the primary differences that I think are useful in understanding it. One is that it could also be called investigative medicine. Sometimes when people ask me what I do, I’ve got lots of answers to this question as you can see, I say I’m a health detective, because people get what that means. It’s kind of a cheeky answer, but it often leads to more conversation.
[00:11:30] They understand the concept of that. It means I investigate what the underlying causes are of a problem. If someone comes to me and they say, “I have IBS,” which means irritable bowel syndrome, I don’t just say, “Oh cool, there’s a drug for that, let me give that to you.” I say, “Okay, so your bowel is irritable. Why is it irritable? Is it because you’re eating gluten and you’re gluten intolerant? Is it because you have too much bad bacteria and not enough good bacteria? Is it because you have a parasite that you picked up while you were on a surf trip in Indonesia? Is it because you are working 80 hours a week and not sleeping, and not managing your stress, and the gut is basically just a big bundle of nervous tissues, which it is?”
[00:12:30] We ask these questions and we address the underlying causes of the problems, and that leads to a much more profound and longer lasting result, so that’s number one. Number two is that it’s patient-centered. What I mean by this is that we treat the patient and not the disease. Let me give you an example. Let’s say two patients come to me and they both have ulcertive colitis, which is an inflammatory bowel condition. In conventional medicine, generally there’s a drug that’s for a condition, and the drug is prescribed to treat the disease. Very little individual attention is paid to the differences between patients that have the same disease.
[00:13:00] Whereas in functional medicine, we’ll look at those two patients, and we might find that they’re actually really different. Even though the ultimate manifestation of their disease is the same, it may have a different cause. For one person it may be primarily stress-related, and thus the treatment is primarily addressing stress. Whereas for the other person, it might be, again, imbalance of good and bad bacteria, or a parasite that’s been undetected, or something else. That person will get a different treatment. It’s really, like I said, about the patient and not about the disease specifically.
[00:14:00] Then the third thing is that functional medicine is restorative. What I’m mean by that is instead of just suppressing symptoms, all of the tests and the treatments in functional medicine are designed to actually promote optimal function, which is where the functional comes from. To actually prevent and even reverse disease instead to just suppressing the symptoms. That’s really a fundamental paradigm shift, and it makes all the difference in the world for patients, and also for clinicians. We feel like we’re actually having a real impact, instead of so many conventional doctors that I talk to who just feel like they’re putting Band Aids on problems, and barely even able to do that with the time that they’re given to spend with patients.
[00:14:30] I just want to emphasize that here, and I imagine there as well, doctors are as much victims of the system as patients are. Most doctors I know got into medicine for all the right reasons. They want to help people, but they are subject to some practice guidelines and ways of doing things that just are not conducive to functional medicine and to this kind of approach. Their hands are tied and there’s very little that many of them can do unfortunately.
Guy
How accepted do you think functional medicine is now today in the general consensus within the medical system? We’re in this bubble, we interview guys like you every week, and everyone’s talking about, “Surely it’s happening everywhere,” but I’m not so sure.
Chris
Yeah no, it’s not. We’ve made tremendous progress in the last few years. One of the biggest headlines is that Dr. Mark Hyman who is, I think, definitely one of the modern champions of functional medicine here in the US. Jeffrey Bland is really the father of functional medicine, I think he even coined the term, but Mark Hyman has done a lot to advance the concept of functional medicine. He was just recently invited to open a center for functional medicine at the Cleveland Clinic, which is one of the most prestigious medical institutions in the world.
[00:16:00] He only recently opened it, but they already have a six month wait list. They already had to move out of the space they were given into an 18,000 square foot facility, so that should tell you something about the demand. From talking with Mark, he said that all of the clinicians, not all, but many of the clinicians, even the quite conservative ones at Cleveland Clinic are showing interest and coming over to talk to him and see what’s going on.
There’s a building interest, having said that, if you probably talked to the average doctor on the street, whether here or in Australia or the UK, I would guess the majority still have not even heard of functional medicine, much less are practicing it, so we still have a ways to go.
Guy
There you go, yeah. Most people are actually just not even looking at it full stop.
Chris
Right.
Stu
How heavily do you look into genetics, and also environmental factors as well as part of that functional medicine practice?
Chris
[00:17:00] That’s a huge part. Arguably that’s all of it, is looking at how genes and the environmental factors interact to contribute to health and disease. There’s a great saying which describes the relationship between genes and environmental factors. It goes, “Genes load the gun but environment pulls the trigger.”
Stu
Yeah, I like it, I like that.
Guy
Could you give some examples of environmental factors as well, yeah?
Chris
[00:17:30] Definitely. We’re talking about diet, sleep, stress management, physical activity, environmental toxins like mercury or BPA, or dioxins, things like that. Social support, play, pleasure; basically when we say environment, another word for this is the exposome, and it refers to the sum of all non-genetic influences that an individual experiences from the moment of their conception. Notice that I said conception, not even birth. The moment when we were conceived, that’s actually when environmental factors start affecting our health, and arguably even before that, all the way through the moment of our death.
[00:18:00] When we’re talking about environmental factors, another way of saying that is, anything that’s not genetics. Anything we’re exposed to that’s not genetic, whether it’s food, air quality, water that we drink …
Stu
Cell phones, all of the above.
Chris
[00:18:30] Pollution, yeah, everything. Getting back to that saying, people often want to know, “How much of health is genetic, how much of it is environmental? If it’s all genetic then who cares? Why do I even bother eating a healthy diet? I’m just going to have fish and chips and drink some beer,” right?
[00:19:00] The thing is, it matters a lot. Even though genes play an important role in determining what conditions were pre-disposed to develop in our lifetime, in the face of environmental triggers, recent estimates have shown that 90% of human disease is driven by environmental factors. What this means is your genes will determine whether you’re likely to go down the diabetes road, or the Alzheimer’s road, or the autoimmune road if you eat a crappy diet and get exposed to a lot of toxins, and don’t sleep and don’t take care of yourself. It’s those environmental factors that actually determine whether you go down any of those roads in the first place.
Guy
They don’t have to express themselves ultimately, the genes.
Chris
[00:20:00]
Absolutely. The environmental factors are what determine whether those genes get expressed or not. The reason that we know this is that we share over 90% of the genes of our distant ancestors and contemporary hunter-gatherers, and they didn’t suffer from these diseases like diabetes and autoimmune disease and Alzheimer’s. They were virtually unheard of in these populations. If a group of people that have the same genes don’t have those diseases, and we have them, it means it’s something in our environment that’s causing those genes to express in a way that leads to those diseases.
Guy
Got it. A question that popped in then Chris is that then, if someone who’s listening to this and they’re like, “Oh crikey, I’ve expressed my genes from my environmental factors over the years, can I un-express them, like turn them off?” What have you seen through your clinic? Is that possible?
Chris
It is and it isn’t. Gene expression is happening in real time, so absolutely that changes even from moment to moment. It’s incredibly complex, and that’s the good news is that choices that we make do effect gene expression in real time, and can have a profound impact on our life.
[00:21:00]
[00:21:30] People know this intuitively. Like if you’re eating really crappy diet, you fall off the wagon, you’re not exercising, and then you start doing those things again, you feel better. Genes are always running the show, so that it’s affecting our gene expression. However, if your genes express in a way that lead to autoimmune disease, for example, as far as we know, there isn’t always going to be a way to reverse that 100% back to the point before that happened. In many situations, it can be reversed to the point where it’s in remission, or the symptoms are so manageable that they don’t interfere with your goals and living a healthy, happy, long life.
[00:22:00]
[00:22:30] No, we’d like to think we have 100% control over everything all the time, but I think we all know that that’s not the case. Sometimes it’s a question of making the best of the hand that we were dealt and the way that our genes have expressed. Which by the way, is not only a result of our choices, it’s also a result of our parents’ and even our grandparents’ choices. That’s either good news or bad news depending on how you look at it, but we now know that choices that our grandparents made and our parents made affected our gene expression while we were in utero and developing. We have, of course, absolutely no control over that. It’s kind of a mixed message where on the one hand, you have ultimate responsibility for all the choices you make which have the biggest impact on your health. On the other hand, you have no say over what your genes are, and how those genes expressed initially.
If you have a tendency, for example, to gain weight, whereas your friend doesn’t, that’s not your fault. It’s just the hand that you were dealt, and it’s something that ultimately you’re responsible for making the best of.
Guy
Bloody parents, eh? They got a lot of …
Stu
Are we that far away from successful gene replacement therapy? I’m aware that there are companies out there now that can zone in on particular issues, and talking about replacements. I don’t really know a lot about it, so I wondered whether you did.
Chris
[00:23:30] I think there’s incredible promise in this field of what’s colloquially called “personalized medicine”. Where we’re looking at genes and gene expression, and we’re looking at drugs and pharmaceuticals that target these genes and can turn them on or turn them off for our benefit.
[00:24:30] I think that we’re certainly going to see some remarkable gains, and ability to cure diseases that have been debilitating and possibly even fatal. In our lifetime, it’s not outside of the realm of possibility that we could see a cure for cancer, or at least really significant progress made there. I’m excited about all those things, and yet, at the same time, they should never take away from the focus on environmental triggers. I think evolution has a way of ensuring that … We’re not just fighting a passive enemy so to speak. These environmental inputs that are not conducive to health, like they mess with us in so many different ways that I don’t think we’re going to be able to solve the problem just by taking pills, no matter how great those pills are.
Stu
Yeah, makes sense.
Guy
Fair enough. Yeah, we’re always looking for the quick fix. Yeah, you’re right, nature’s going to have a way of intervening along the way I think. Talking about environmental factors, I know you spoke about the four pillars of health, breaking that down. I was wondering if you could touch on them for us a little bit, please Chris.
Chris
[00:25:00] Yeah sure. This is something I’ve thought a lot about because I wanted to … People would often ask me at conferences, or speaking events or whatever, “I’m so overwhelmed. I want to feel better but I don’t know where to start. Where can I have the biggest impact? If I focus my energy just on a few things, what should that be?”
[00:25:30] When I looked at the research and thought about my own experience, and also treating thousands of patients now, the four pillars that I came up with were nutrition, sleep, physical activity, and I’m purposely not saying exercise, I can explain why in a second, and stress management. I think if people dial in and really get those four things dialed in, we could probably address 80-90% of disease with those four pillars.
Stu
If I said to you, “Chris, I love this, you’ve got four pillars, but I’m so busy. I only have time for one pillar,” which pillar [crosstalk 00:26:06]?
Chris
[00:26:30] That’s a tough one. I think if you think about it in terms of triage, it would be sleep. Obviously if you don’t sleep, you can not eat for a long time, months at a time and still survive. You can eat a crappy diet and still survive, but if you don’t sleep for three nights or four nights, you’re dead. Sleep has got to be really far up there at the top of the list, but on the other hand, if you eat a crappy diet, it’s probably going to interfere with your sleep. It’s really hard to do that with these things because they’re all so inexorably intertwined with each other. It’s either a positive feedback system where they’re all reinforcing each other, or it’s a negative feedback system where they’re all breaking each other down basically.
Guy
Fair enough. I reckon if you go on top of three of them, the fourth one would kick in anyway if you were managing it. That’s how I would see it.
Chris
One would hope.
Stu
One would hope, absolutely.
Chris
[00:27:30] I’ll tell you the one that gets left out the most, and that’s stress management. I have lots of patients who’ve got their diet, and sleep, and physical activity pretty wired. They understand the importance of addressing all those things, but they really don’t pay attention to stress management. I think that’s often the elephant in the room for when I’m treating patients, and just for people in general. We live in a culture that really doesn’t value that. The dominant paradigm is just more, faster, more intense. I know most people that I know feel really spread super thin. They’re burning the candle at both ends and they’re not doing anything to manage that stress. I think that’s the biggest mistake that I see.
Guy
What would you advise that person that comes into your clinic, Chris?
Chris
[00:28:30] I would say pick some practice, whether it’s meditation, or yoga, or deep relaxation, or spending time in nature. Whatever it is that has the biggest impact for each person, because it’ll be different from person to person, and commit to doing it, but don’t over-commit. Just commit to five minutes a day as a starting place. What happens is, you’ll be much more able to follow through with that commitment. You’ll start to experience some of the benefits of it, and then you’ll gradually be able to increase it over time.
[00:29:00] There are some really helpful apps now, like for meditation, like Headspace, that can really help people to acquire this new habit until it becomes something like brushing your teeth. Where, if you’re tired, you still brush your teeth because you know it’s good for your teeth and you don’t want your teeth to fall out. Like, it’s time to sit on the cushion and meditate and you don’t feel like it, you still do it because you know that doing it is an important part of your overall health and well-being. It has to become a habit like that and be integrated into our life, but it doesn’t start that way. You have to start small and build up slowly.
Guy
Like everything, yeah, fantastic. Do you meditate daily, Chris?
Chris
Yeah. My dad, I love him and he’s been an incredible dad. One of the greatest gifts I received from him is him introducing me to meditation when I was 17. He didn’t stick with it for very long, but in stayed with it for 25 years now. It’s been a regular part of my life, and it’s helped me get through some … It’s been a stabilizing presence, and something I couldn’t imagine not doing at this point.
Guy
Incredible.
Stu
I wanted to raise the subject, topic of gut health. You spoke about your four pillars, and how if you get these pillars wrong, then I guess the foundation collapses. Gut health is such a buzz word that ten years ago it seemed to be quackery, but now it almost seems to be the epicenter of health. How important is the consideration of our own personal gut health, from your perspective?
Chris
[00:31:00] I think it’s vitally important. What’s interesting is this has been known for a long time. Hippocrates 2500 years ago said, “All disease begins in the gut.” Which is really remarkable considering that he had no modern investigative tools, or diagnostic procedures, or anything. It’s taken us two millennia to actually confirm that he was right with modern science, and investigative tools that we have available to us now.
[00:31:30] If you look in the scientific literature, there isn’t really a day that passes where there isn’t a connection drawn between some condition that most people would have no idea has anything to do with the gut. Like Parkinson’s Disease, Alzheimer’s, diabetes, heart disease, eczema, psoriasis, other skin conditions, Hashimoto’s, which is an autoimmune thyroid problem, anxiety, depression. Every day there are studies that show a connection between these disparate conditions and gut health.
[00:32:00] Does that mean gut health is the only thing that is driving those conditions? No, I don’t think so, but it does mean that our gut is crucial to our overall health. If we don’t address our gut health, that can be a real risk factor for not just gut problems, but problems all around the body.
Guy
Yeah, wow. How accurate is gut testing to show up? How successful can we, in turn, that [inpermentability 00:32:17] around, or whatever might be going within the gut on to …
Chris
Yeah, those are both good questions. The answer depends on what kind of tests are run. With gut testing, you can look at stool. You can do stool testing, you can do breath testing, and you can do urine testing, and they all provide different kinds of information. Of course you can do colonoscopies where they’re actually looking at the tissue itself, or endoscopies where they put a tube through your throat. There’s other kinds of testing, but that kind of testing is really designed to detect structural problems. Like the kind of testing you would get from your gastroenterologist, where they’re putting tubes in you in both ends.
[00:33:30] That only really is designed to detect structural issues. Like if you have inflammation in your gut that’s related to Crohn’s Disease, or ulcerative colitis. In some cases it can find some bacterial infections in your stomach like H. pylori, like bacterium that causes ulcers. Two Australian physicians, by the way, discovered that. Everyone used to think ulcers were caused by stress, but two Aussie physicians found out that no, actually this bacterium H. pylori is the underlying cause in many cases.
[00:34:00]
[00:34:30] The tests that we do in functional medicine are, as the word would suggest, more functional. They’re designed to detect imbalances that don’t necessarily affect the tissue, but they’re still driving a lot of problems. For example, a lot of people have probably heard of the microbiome, which is the collection of microorganisms that inhabits our gut and other parts of our body. We now know that these microorganisms play a profound role in health and disease. If you have too many bad bacteria and not enough good bacteria, that’s going to cause a problem.
In the conventional medicine world, they don’t really test for that. If you go see your gastroenterologist, they’re not typically going to be looking at things at that level. You’ll have to find someone who practices functional medicine, or has that orientation and knows how to do that kind of testing, in order to figure out what’s going on there.
[00:35:00] Fortunately there are more training programs now for functional medicine for clinicians. I have a training program, Institute for Functional Medicine. There are several Australian physicians in my program right now, and we just enrolled a few more for the next group. I think it’s hard to find someone now, but that’s going to be changing in the next few years.
Guy
[00:35:30] Yeah, brilliant. I have another question popped in there as well along side that, is candida. It’s something that we can hear quite often. What is it, how much of a problem is it? Do you see it with your clients and patients?
Chris
[00:36:00] Candida is a yeast, and everyone has yeast in their gut. I think candida can be a real issue, but I think it’s one of these things that went from being quack diagnosis to fad diagnosis. A lot of people were looking at checklists of symptoms online and diagnosing themselves with candida overgrown just on the basis of a questionnaire on the Internet. I don’t think that that’s evidence-based, or a good way of going about things.
[00:37:00] I think that candida has become somewhat overblown, or at least it did in the early 2000s. There is a real possibility if the gut microbiome becomes out of balance that some fungal organisms that live in the gut could become overrepresented and cause problems. Even though we all are supposed to have some fungus in our gut, we’re not supposed to have a lot. If candida that is naturally there and not causing any problems, it’s really overgrown, that could be an issue. That can be detected with these functional medicine tests, and if someone suspects that they have candida, it’s probably best to confirm that with that kind of testing, if possible.
Guy
Got it. Last question Stu, sorry.
Stu
You’re stealing the show, Guy. Carry on.
Guy
We spoke about testing and then actually turning these issues around.
Chris
Oh right.
Guy
[00:37:30] Yeah, just bring that into it as well. Is it difficult, so if somebody comes in and all the markers are showing, like, “Oh my God, the state in the gut is shocking,” how hard is it to turn around? I know it’s not something you can do in a couple of weeks.
Chris
[00:38:00] Yeah. That’s true, it’s not something you can do in a couple of weeks, typically. Although in some cases, if someone has a parasite and the protocol is effective, it could actually turn around that quickly. Usually it takes weeks or months, and the first stage is identifying what’s wrong. That, to be honest, can be the toughest stage for a lot of people, especially if they don’t have access to a functional medicine provider.
[00:38:30] Then once you find out what’s wrong, you can break it into two stages. The first is addressing the pathogen if there’s a pathogen present, like an infection or a bacterial overgrowth in the small intestine. Then the second stage is rebuilding a healthy gut ecosystem. That’s really what the gut is, it’s an ecosystem. Once you eradicate the pathogen, that’s only generally the beginning of the recovery. You got to get rid of that thing that shouldn’t be there, but then you have to rebuild the environment to be an environment that would resist future invasions, and also just one that functions well and digests nutrients, and absorbs them effectively. It’s a two phase process.
Stu
I wanted to draw the connection, Chris, between the gut and the brain. It seems to me that there is almost an epidemic now of neurodegenerative diseases that are starting at a much earlier age. I wondered what we could do, in your opinion, to start to safeguard ourselves as soon as we can, where our brain health is concerned?
Chris
[00:39:30] Yeah, that’s a really big issue now. It’s starting in childhood with things like ADHD and autism spectrum disorder, and OCD, and increase in all of those cognitive, behavioral, emotional disorders. Then we’re also seeing it in adulthood with a rise in the prevalence of Alzheimer’s and Parkinson’s and other neurodegenerative conditions.
[00:40:00] When it comes to ways to die, those are pretty low on everyone’s list. Alzheimer’s is a scary condition that wreaks havoc on families and caregivers in addition to devastating the person who has it. I think most people if they could choose would much rather just have a massive heart attack and check out that way then have a long and slow …
Stu
Be done.
Chris
[00:40:30] Yeah. It’s a problem, and it definitely is on the rise. It’s not just due to increased rates of detection, whether you’re talking about autism or Alzheimer’s. You already mentioned half of it. We talk about the brain health; you can’t talk about brain health without talking about gut health. There’s a bi-directional relationship between the gut and the brain, which means that the health of our gut is going to affect the health of our brain, and the health of our brain affects the health of our gut. They’re a two way street for communication between those two organ systems.
[00:41:30] In fact, the most recent theory on what causes depression is that it’s not so much an imbalance of neurotransmitters, but it’s, they call it the inflammatory cytokine model of depression. Where inflammation in the gut actually then suppresses activity in the frontal cortex in the brain, and leads to the symptoms of depression. This is not a fringe theory, this is in mainstream medical journals right now, and many researchers believe this is probably the primary cause of depression. If it’s the primary cause of depression, we also see studies that correlate bacterial overgrowth in the small intestine with Parkinson’s, all kinds of GI issues with all kinds of brain problems.
[00:42:00] That’s one thing, and then the other, in terms of protecting brain health above and beyond the gut, the brain is one of the most resource-intensive organs in the body. It needs a lot of energy, it needs a lot of micronutrients like iron, zinc, folate, vitamins A, B12, B6, C, D, K2, and then DHA, which is a long chain omega-3 fat. Our diets have shifted from being very nutrient-dense with a lot of these nutrients, to being, and energy-poor, meaning high in nutrients and low in calorie, to the opposite of that. Now we eat lots of calories with very few nutrients, and that’s really bad for brain health.
[00:43:00] Then you’d want to do everything that you can to reduce inflammation, because inflammation is like Kryptonite for the brain. That would include an anti-inflammatory diet, but it would also include addressing any underlying issues, like gut issues that we’ve been talking about, and then dealing with more of the lifestyle factors that can lead to inflammation. Physical inactivity, most people don’t think of it this way, but being sedentary is actually inflammatory for the body. Not getting enough sleep causes inflammation. Not managing your stress causes inflammation.
People wonder why those four pillars are important. One of the reasons is that they’re all anti-inflammatory, and inflammation is the root of all chronic modern disease. Anything we can do to reduce inflammation is going to reduce our risk for modern disease.
Guy
Got it, that’s a great answer.
Stu
Fantastic.
Guy
Another thought that popped in there Chris, they’re just coming from everywhere today, don’t know what’s going on. You talk about the nutrient-dense diet, and we lack in vitamins and minerals. If we haven’t addressed our gut in the first place and we do have leaky gut or things are not going on right, what happens? How effective is eating nutrients, or are they going to just bypass us?
Chris
I think it’s another one of those two way streets, chicken and egg kind of problems. For example, zinc is required, promotes healthy-tight junctions, which means it keeps the gut from being leaky. If you don’t have enough zinc in your diet, your gut can become more leaky, and then eating foods that are richer in zinc can help your gut to recover.
[00:45:00] Having said that, absolutely, if someone has mal-absorption and bacterial overgrowth in their small intestine, the small intestine is a place where nutrient-absorption happens. You’re not supposed to have a lot of bacteria there. The reason for that is the bacteria like the same nutrients that we need. If you eat nutrient-dense food, you got a lot of bacteria in your small intestine, guess who’s going to get to that food first? The bacteria, and you’re not going to get as much of it. Absolutely it is important to address those pathologies, but that’s not an excuse for people not to eat a nutrient-dense diet if they have one of those pathologies.
Stu
[00:45:30] No, that makes sense. Given the fact that I’m going to be proactive in addressing the pillars, and I’m going to do everything I can, but I really love bread. Gluten is, again, another one of these buzz words. Everybody bashes gluten, seems to be part of so many diets that are quite health-giving as well, like the Mediterranean diet. What’s your take on it?
Chris
[00:46:00] I’m maybe a little bit more moderate than some other people in my field, and maybe more aggressive as well, at the same time. I think that gluten intolerance is far more common than is conventionally recognized. In the conventional world, most doctors would say, “Oh, celiac is rare, it only affects less than 1% of the population. If someone doesn’t have celiac, then they don’t need to worry about gluten.”
[00:46:30] I think that is completely false. It’s been demonstrated with a lot of peer-reviewed research now that there’s a condition called non-celiac gluten or wheat sensitivity, where people who don’t have celiac react to wheat and gluten, and quite strongly and significantly in many cases. It can be as severe as the reaction that some celiacs have. It’s associated with an increased risk of disease and an early death.
[00:47:30] Unfortunately that’s really not on the radar for a lot of clinicians, and they’re not actually testing for it. Then there’s even, with celiac, the number of people that are undiagnosed outnumber the people that are diagnosed by up to six to one. There are a lot of people with celiac disease out there who have no idea that they have it. They may not even have significant gut symptoms, and they call this silent celiac disease. It’s a form of celiac where they don’t have the diarrhea when they eat wheat that a lot of people have. That’s in some ways even more dangerous, because they go on eating gluten and wheat, and they way it manifests for them is that they have a massive heart attack when they’re 55. No one ever even knew that that was connected because they were never actually tested.
[00:48:30] That’s the one side, that I think it’s under-recognized, under-diagnosed. On the other side, even the most liberal estimates of how many people are gluten intolerant, I’ve never seen anything that is higher than 10%. That means 90% of people are not gluten intolerant, which is the majority of people of course. Does that mean we should all eat bagels for breakfast, and sandwiches for lunch, and cookies for dinner? Not necessarily, because if you think about the foods that gluten tends to be found in, what are they? They’re bread, crackers, cookies, beer. Highly-refined, highly-processed, nutrient-poor foods in general.
[00:49:00] What I tell people is, “Look, if you know you’re not gluten intolerant, you’ve been tested, eat a nutrient-dense diet. This will be low in gluten generally, but if you want to go out to a restaurant and have a piece of bread, or have a drink of beer, something like that, great. If you can do that 20% of the time and follow the diet that you should be eating 80% of the time, then I think that’s a good balance. If you do that and you feel well, and you feel healthy, and you don’t feel wrecked the next day after you’ve had that piece of bread, and you feel just the same, then I think it’s pretty hard to make an argument against that kind of approach for someone who’s otherwise healthy.”
Stu
Makes perfect sense.
Guy
[00:49:30] I’m aware of the time Chris, and I know we’re going to run out of time soon. I wanted to quickly mention physical activity. Obviously you’re in front of a computer quite often, and see patients and things like that. How do you handle your day and incorporate that movement, and avoid the inflammation, sedentary lifestyle.
Chris
I’m not sure if you can see my treadmill down there.
Stu
Oh, yes.
Guy
Ah.
Chris
I have a treadmill desk, which is a step up from a standing desk. I actually walk when I’m writing, or sometime when I do phone consults from my home office here, or if I’m just emailing or whatever. Generally I take meetings on the treadmill desk. I don’t do them for podcasts because the treadmill makes noise, and kind of irritating in the background.
[00:51:30] When I say physical activity, I phrase it that way instead of exercise, because studies have shown that if you’re sedentary most of the day, and even if you go to the gym three or four times a week and get the recommended amount of exercise, you’re still at increased risk for disease and early death. It’s really important to approach physical activity from two different directions. One is, yes, we do need to exercise, the research is solid on that. Getting moderate to higher intensity activity regularly throughout the week is crucial, but on the other end, we also have to reduce the amount of time that we spend sitting. Humans we’re just not designed to sit for long periods, and that means standing. Ideally standing for up to half the day, varying your sitting and standing, and walking somewhere between, ideally around 10,000 steps a day. If we can walk 10,000 steps, stand at least half the day, and do exercise throughout the week, then we’re mimicking what the natural human template of physical activity is, and we dramatically reduce our risk of disease and early death.
Guy
Got it, brilliant. Like that idea.
Chris
[00:52:00] Just a word on that, because some people might hear this and get discouraged because they’re like, “I work in an office and my boss isn’t going to be cool with me getting a treadmill desk, so what am I going to do?” In my book I talk about some different strategies. They include things like riding your bike or walking to work if that’s possible. Even if you have to drive to work, you can park a mile away from your office so you can walk at least that mile, or if you take public transport you get off a stop or two away from your office so you walk.
[00:52:30] You take walking meetings at work. If you have to have a meeting with someone you say, “Hey, let’s go outside and go on a walk.” You can stand at meetings. You’ll be that irritating guy or gal standing, but just tell them you have a back problem, it works every time. You take the stairs every chance you get instead of the elevator. There are a lot of ways you can work this physical activity in if you have that mindset.
Stu
Good advice.
Guy
Yeah, thank you Chris.
Stu
I need to stand up.
Guy
Yeah, well I’m standing. Last question we ask everyone on this show. What’s the best piece of advice you’ve ever been given?
Chris
Yeah, that’s a tough one. There’s so many ways we could go of spiritual health, business, relationship. I think if we keep it general, I like the rocking chair test. Which is, when I have a big decision to make, or I’m thinking about what’s important and how I want to spend my time, really thinking about the bigger questions in life, I imagine that I’m in a rocking chair at age 100, if I’m lucky enough to make it. I look back on my life, and I think, “What would I wish that I had done more of? What would I not care about, from that perspective? What would seem important and unimportant?”
[00:54:00] It seems like a kind of cheap trick, but it actually is really powerful in terms of clarifying what my purpose is, how I want to spend my time, and what I want to devote my life to. For me, when I’ve done that test repeatedly, there are a few things that always percolate to the top of the list. I’m constantly reorganizing my life to focus on this, and one is being the best dad that I can be. I have a five year old daughter, and being present for my daughter and family, that’s always at the top of the list and trumps everything else.
[00:54:30] Then doing what I can to contribute to a healthier, happier world. Helping people to recover their health and live their dreams, which is something that is very personal for me obviously because of my past and history, and where I think I can make the biggest contribution.
Guy
Fantastic.
Stu
Brilliant.
Guy
You’re clearly doing that Chris, that’s brilliant, mate. We haven’t even mentioned, you’ve got a rocking podcast, like it’s amazing. You’ve got a wealth of information on your website as well, you’ve got a book. If people want to get more of Chris Kresser, and this is the first time they’ve been introduced to you, where do you recommend they go, mate?
Chris
Yeah. There’s two places to find everything. One is chriskresser.com, so that’s my blog, and there’s lots of education programs for people, consumers, and also a link to my podcast is there. Then kresserinstitute.com is the website that has all the information for clinicians that want to learn about functional medicine, and this approach to health and medicine that we’ve been talking about on the show. I have a training program for doctors and other healthcare professionals that are interested in this approach, and you can get more information about that there. It’s a distance learning program, so we have physicians and other clinicians in Australia, New Zealand, UK, Europe, Canada, South America, and of course the US. It’s a great group of people.
Guy
Fantastic.
Stu
Fantastic, we’ll put it all in the show notes and make sure that everyone knows.
Chris
Great guys, happy to meet you both.
Guy
yeah, thanks so much for coming on the show.
Stu
Yes, thank you mate, and look forward to following your journey as well.
Chris
All right, take care guys too, good to meet you. Bye.
Guy
Thank you.
Stu
Thank you, bye bye.
How did we do?
If you rate this transcript 3 or below, this agent will not work on your future orders